

Learn about RSTACK Solutions' Comprehensive Applications, Consulting, Infrastructure, Cloud, and BPO services

Our application services provide you with the tools and technology you need to streamline your operations...


Our cloud services offer a flexible and scalable infrastructure to support your growing business needs


Our consulting services provide expert guidance and support to help you achieve your business goals

What is Provider Credentialing?
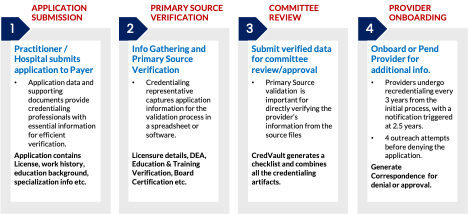
Provider credentialing in healthcare refers to the process of validating the qualifications, licenses, and certifications of healthcare professionals to ensure their capability to deliver high-quality care to patients. This important requirement for healthcare organizations is overseen by regulatory bodies such as the federal Centers for Medicare & Medicaid Services (CMS) and the Joint Commission on Accreditation of Healthcare Organizations (JCAHO)
What is CredsVault?
Simplify Provider Credentialing with RSTACK's CredsVault! Our streamlined solution takes the hassle out of the credentialing process. Credsvault grants you access to 1.4 million verified healthcare provider records. We meticulously verify education, licenses, experience, certifications, affiliations, malpractice history, and adverse clinical occurrences, delivering a comprehensive and reliable provider information packet for committee review and approval. CredsVault revolutionizes traditional manual processes by connecting all stakeholders on a unified platform. Enjoy the benefits of customizable e-applications, efficient document management, and personalized dashboards. Our paperless work environment and automated solutions not only save time but also enhance turnaround time (TAT).
Enhance Member Satisfaction with RSTACK CredsVault's Accurate Provider Directories!
When it comes to selecting healthcare providers, accurate provider directories are essential. With our provider directory management feature, Credsvault ensures plan compliance with CMS regulations and enhances the member experience through real-time updates and validated information. By maintaining up-to-date and reliable provider directories, CredsVault empowers members and patients to make informed decisions about their healthcare choices. They can confidently choose their preferred providers, knowing that the information they rely on is accurate and trustworthy.

Customizable E-Application
Customizable Dashboard
Document Management
Provider Directory Management
Initial Credentialing & Re-Credentialing
Custom Reporting
Re-Credentialing Queue with QC Queues
Workflow Automation
Multiple Integration Capabilities
Automated Notifications & Correspondence
Customized FAQs
Improved TAT
Compliance with Regulations
Accurate Provider Directories
Improved Star Rating
Reduced Denials
Access to Information
Reduced Manual Efforts
Reduces Re-work
Reduced call volumes
Automate Outreach efforts
Promotes Automation

MemberDesk is the perfect solution for health plans that want to improve member engagement and enrollment. Contact us today to learn more about how MemberDesk can help your health plan.
Choose CredsVault by RSTACK Solutions, your trusted partner in provider credentialing. Streamline your credentialing process, ensure compliance, and enhance provider and member satisfaction. Experience the power of automation and accuracy with our customizable features and comprehensive solutions.
Ready to simplify your provider credentialing?